Mpox (monkeypox)
What You Need To Know

If you are fully vaccinated (received two doses of the mpox vaccine) or have previously had mpox, you are considered protected against severe illness from both Clade I and Clade IIb. However, if you have only received one dose of the vaccine, you are not fully protected. It is strongly recommended that you receive your second dose as soon as possible. Booster shots are not currently recommended.
Click here for more information on current mpox vaccination availability.
**The information on this page below relates to the mpox outbreak of IIb that disproportionately affects gay and bisexual men. The current global and national mpox situation is changing rapidly and guidance is likely to change as the situation emerges.**
Mpox, the new name for monkeypox: In line with the recent World Health Organisation recommendation, we are updating all of our resources and webpages to ‘mpox’, the new term for monkeypox.
What is mpox?
Mpox is a viral infection. It can lead to an illness that ranges from mild to severe and can last a number of weeks. Up until recently, it was only seen in countries where the virus is endemic (very common) and sometimes in people who return home from those countries. However, the 2022/23 outbreak in non-endemic countries is primarily seeing the virus spreading among sexual networks of gay, bisexual and other men who have sex with men (gbMSM) through close contact with someone that has mpox. Most people are not seriously unwell with mpox but some can experience intense pain. Serious illness is more likely in those with a weak immune system, pregnant people and young children. So far, in non-endemic countries, mpox is rarely fatal, however, people have died during this outbreak – no deaths have been recorded in Ireland.
How do you get mpox?
Mpox can be passed on from person to person through:
- Very close contact with a person that has a mpox skin rash, blisters, ulcers or scabs. This includes any kind of sexual contact (oral sex, anal, vaginal/frontal) and intimate contact (kissing, cuddling, holding hands).
- Contact with clothing, bedding, towels, etc that have been used by a person who has monkeypox.
- Breathing in droplets from the coughing or sneezing of someone who has monkeypox.
What are the symptoms?
Initial symptoms of mpox usually appear within 5 to 21 days of being exposed to the virus. Symptoms include:
- fever (of 38C or higher),
- headache,
- muscle aches,
- backache,
- swollen lymph nodes,
- chills & exhaustion.
- pain or bleeding from your rectum (bum)
An important symptom to remain alert to is an unusual rash, spots, blisters, ulcers or scabs. These can occur on any part of your body but many of the people in this current outbreak are developing the spots in or around their genitals, bum or mouth. The spots go through a number of stages (see pictures below). Starting as raised red spots, which turn into small blisters that are filled with fluid. The blisters eventually begin to form scabs which later fall off.
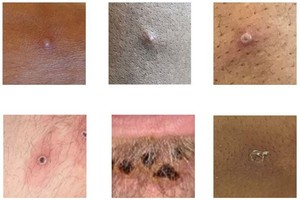
Additional images of the different stages of the rash can be found on the HPSC website here.
What is the illness like?
Mpox is usually a self-limiting illness, meaning most people will recover from the virus themselves at home within a few weeks.
Most people are not seriously unwell with mpox but some can experience intense pain. Serious illness is more likely in those with a weak immune system, pregnant people and young children. Very few people in Ireland have been hospitalised with mpox. So far, in non-endemic countries, mpox is rarely fatal, however, people have died during this current outbreak – no deaths have been recorded in Ireland.
What is the risk?
This outbreak is disproportionately affecting gay, bisexual and other men who have sex with men (gbMSM). Cases of mpox are being diagnosed each week in Ireland, most but not all are happening in Dublin. As mpox is passed on through very close contact with the lesions of a person with mpox, sexual contact (oral sex, anal, vaginal/frontal) and intimate contact (kissing, cuddling, holding hands) pose a considerable risk. To learn more about making informed choices about your sex and social life during the mpox outbreak, click on the image below.
It is important to know that we are still learning about how mpox is transmitted and how it affects us. As we understand more about what puts us at risk of getting mpox, we’ll share it with you here and on social media.
How can I make sex safer during the mpox outbreak?
Sex is an important part of the lives of many of us. We know that during this outbreak people are going to continue having sex, so we’ve some suggestions on how to make sex safer, if you choose to have it. Click the image below to read our monkeypox safer sex suggestions.
It is important to know that we are still learning about how mpox is transmitted and how it affects us. As we understand more about what can make sex safer from mpox, we’ll share it with you here and on social media.
Can I get vaccinated against mpox?
For all you need to know about the mpox vaccine in Ireland, visit our mpox vaccination page here.
When to seek medical help?
If you are experiencing what you think might be the symptoms of mpox contact your local sexual health clinic or GP (general practioner / family doctor) to discuss your symptoms. Do not attend a clinic or your GP without calling ahead first so that they can be prepared for your arrival and offer you the best care. To find the details of your local sexual health clinic contact our outreach team.
If you need to be seen by a doctor, they will organise an appointment for you and will give you advice on how to get to the clinic. In the meantime, keep your distance from other people and do not engage in sexual contact until you have been seen.
Where can I get support, if I need it?
The MPOWER team is available to offer you information and support on all things sexual health, including mpox. You can call us, text us, Whatsapp, email, Zoom or find us on Grindr and other hook-up apps. Full contact details are available here.

We have also launched a free counselling service, available to anyone who would benefit from time and space with our MPOWER psychotherapist to discuss a mpox diagnosis or the impact the outbreak is having on your mental, sexual or social health. 6 sessions are available free-of-charge and will take place online via zoom.
To self-refer for this service please email mpower@hivireland.ie with a first name and contact mobile number. A member of the team will make contact you to set up an appropriate day and time to start the sessions.
Where can I get more information?
It’s important to get information from a reliable source such as the Health Service Executive (HSE) or Health Protection Surveillance Centre (HPSC). At MPOWER, we are working with these agencies on the response to mpox with our partners in the Gay Health Network. We’ll be updating the information on our website and through social media as the situation changes.
Health Protection Surveillance Centre – Monkeypox